When Pearland resident Sue Gordon experienced irritation on the roof of her mouth, she went to her dentist.
“I had felt some discomfort on occasion, but it was never seriously painful,” she said. “I’d had a biopsy done over a year ago and the report came back as benign. Still, I felt it was important that I get a more definitive answer.”
Sue’s dentist examined her mouth and noticed that a protrusion had begun to form at the site of the irritation. Concerned with the finding, she was referred to an otolaryngologist who performed another biopsy.
“Though the pathology report came back again as benign, the physician told me he didn’t like the look of the result. He recommended that I speak with someone from oral and maxillofacial surgery at UTHealth Houston,” she said.
Sue met in July 2019 with doctors from UTHealth Houston Oral and Maxillofacial Surgeons, who examined the affected area, which now was showing a mass and signs of bone loss along her upper jaw. After some analysis and discussion, the doctors advised that a more comprehensive biopsy be completed.
For Sue’s initial procedure, she was referred to Mark Wong, DDS, professor and Bernard and Gloria Katz Endowed Chair in the Department of Oral and Maxillofacial Surgery at UTHealth Houston School of Dentistry. The procedure was successful in identifying that the mass was a rare form of cancer.
Sue was then referred to Jonathan Shum, MD, DDS, oral and maxillofacial surgeon and associate professor at UTHealth Houston School of Dentistry.
“After meeting with Sue and learning about her condition, our team came up with a planned, multi-procedural approach for treatment. Surgery to remove the cancer was scheduled, which involved removing the remaining upper jaw and palate, followed by testing and monitoring to ensure the treated area was clear of any cancer or return of infection,” Shum said.
Working with restorative dentistry and prosthodontics expert Joann Marruffo, DDS, a temporary upper denture was created to make Sue as comfortable as possible before her next procedure.
“I’d had some fear the cancer would come back and spread elsewhere in my body. I was glad to know the surgery was successful,” Sue said. “No matter what questions I had during the process, they never discounted them. It really helped me keep a positive attitude, along with a little praying.”
Given the extent of procedures Sue had already experienced, Shum felt she managed her treatment well.
“Given the extensive nature of Sue’s surgeries, a major concern for me was her comfort prior to the rebuilding procedure. With no upper jaw and relying on a denture for several months, simple oral functions were naturally a major challenge,” Shum said. “The way she handled it all really demonstrated a great deal of perseverance and positive spirit.”
The next step would focus on the reconstruction and rebuilding of her upper jaw using a free tissue transfer, or free flap. The procedure involved the transplant of the fibula bone, skin, and blood vessels from the lower leg to reconstruct the upper jaw and palate. Specialized hardware was also designed to hold the transferred tissue in place, plus dental implants for adding a prosthesis for the replacement of Sue’s teeth.
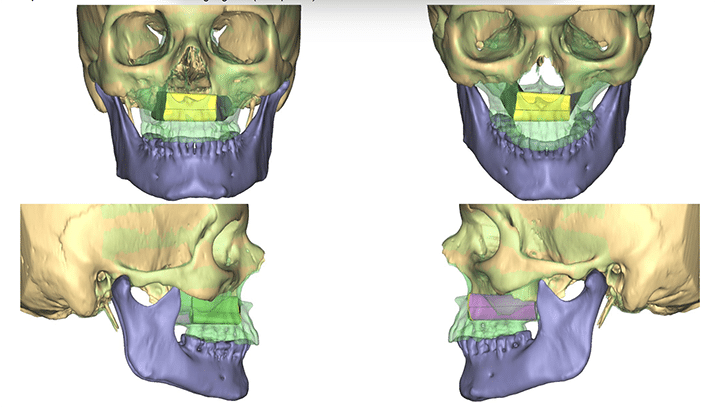
With the assistance of Nagi Demian DDS, MD, professor and Thomas M. Weil Professorship in Oral and Maxillofacial Surgery at UTHealth Houston School of Dentistry, intraoperative navigation techniques were utilized to ensure the reconstruction went exactly as planned, allowing for the placement of the dental implants created for Sue’s new teeth.

Sue has continued appointments and consultations with Shum and other doctors to check on her progress. Along with additional grafting procedures, she has been able to replace the lip tissue and structure that was removed in the earlier surgeries.
For Shum, he is just pleased to have been a part of Sue’s treatment and restoration.
“While Sue’s rehabilitation was long and remains ongoing, I believe the end result ultimately brought a significant change,” he said. “I’m thankful to have been a part of bringing healing and normalcy to her life.”



