Empty Nose Syndrome
Empty Nose Syndrome
Empty Nose Syndrome is a rare complication of nasal surgery with symptoms including trouble breathing, headaches, and pain. UT Physicians is here to help you receive recognition and relief.
Empty Nose Syndrome is a rare complication of nasal surgery with symptoms including trouble breathing, headaches, and pain. UT Physicians is here to help you receive recognition and relief.
Take Our Empty Nose Syndrome Assessment
Have you ever had surgery on your nose, including your septum and/or turbinates?
You may want to consider another treatment. Please visit our Nasal Airway Remodeling page for additional help.

Click “Start Assessment” below for a short screening survey. Using the provided numerical scale, your points will be added up at the end of the quiz.
Rate your symptoms on a scale from 0-5:

0 No Problem
1 Very Mild
2 Mild
3 Moderate
4 Severe
5Extremely Severe
Start AssessmentYour Score:
What are turbinates and why are they important?
Nasal turbinates are part of the nasal cavity that help us adjust the humidity, temperature, and speed of the air we breathe through our nose. In some people, they can grow too large and severely impact airflow. Surgery to shrink turbinates is very common and often done in combination with straightening the nasal septum to improve breathing.
What can happen if too much turbinate is removed during surgery?
Turbinates work hard to perfect the air we breathe in and sense how well it is flowing through our nose. Losing too much turbinate can leave your breathing feeling dry and uncomfortable in your nose and throat. This can lead to other symptoms such as congestion or shortness of breath.
Augmentation Turbinoplasty
In an abstract presented at the American Rhinologic Society meeting in May 2024, Martin J. Citardi, MD, a rhinology specialist and a professor and chair of the Department of Otorhinolaryngology-Head & Neck Surgery at McGovern Medical School at UTHealth Houston, analyzed the use of bovine-derived collagen matrix (BDCM) in inferior turbinoplasty procedures performed on patients with empty nose syndrome.
“To date, there’s no study looking at the use of BDCM in this group of patients,” says Citardi, who’s also vice dean for clinical technology at UTHealth Houston. “Our data confirm this is a suitable grafting material with good, long-term results.”
Patients who underwent the procedure using the bovine-derived matrix reported significant improvement in nasal dryness and crusting, feelings of suffocation, the feeling of the nose being too open, and any burning sensation.
“Our retrospective review confirmed our impression that these patients have had a sustainable and durable positive response,” he says. “The matrix is easy to manipulate, doesn’t become infected, and seems sustainable. We’re also avoiding the second incision and healing time required with an autograft. As awareness of the condition increases, we expect to see more patients needing treatment.”
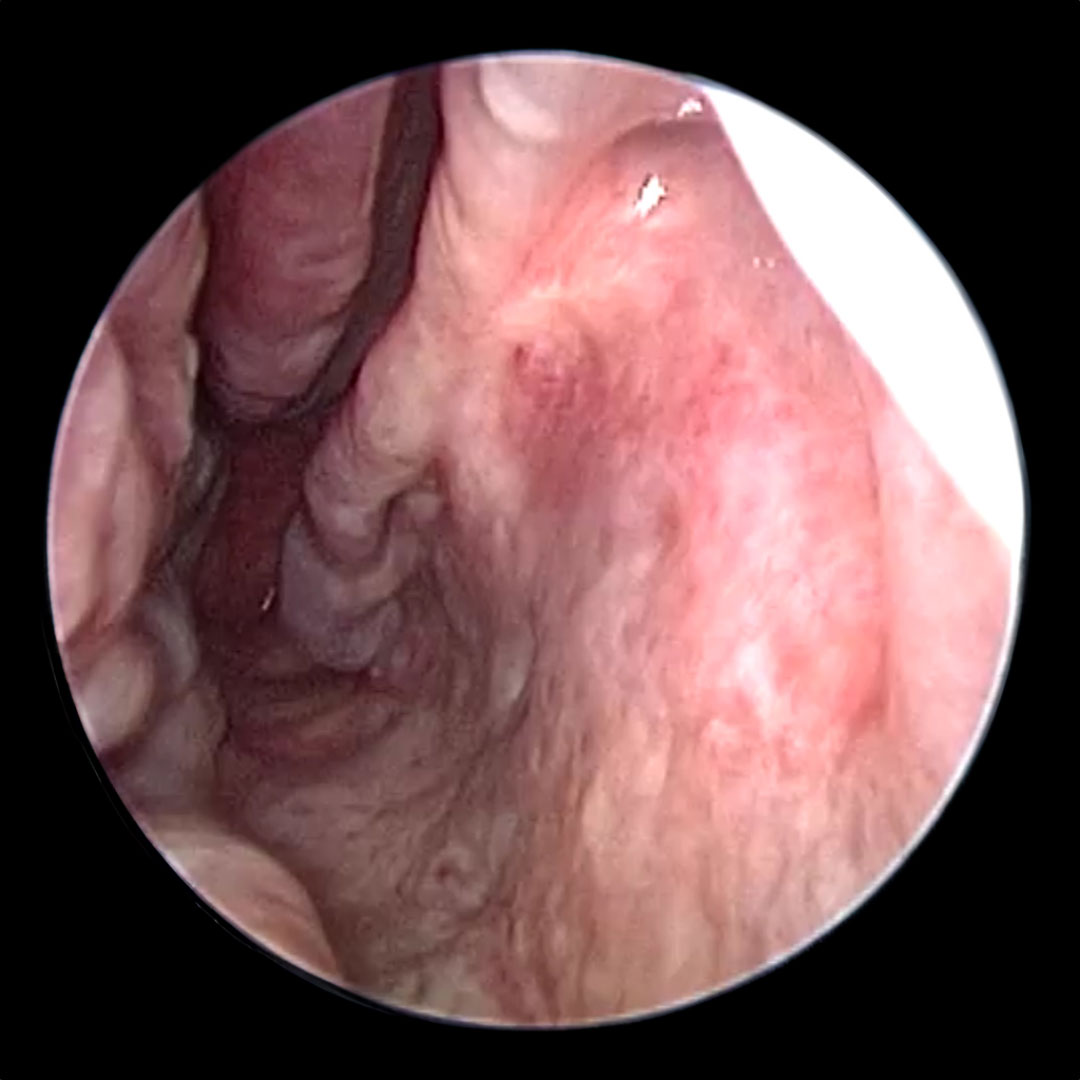 Before
Before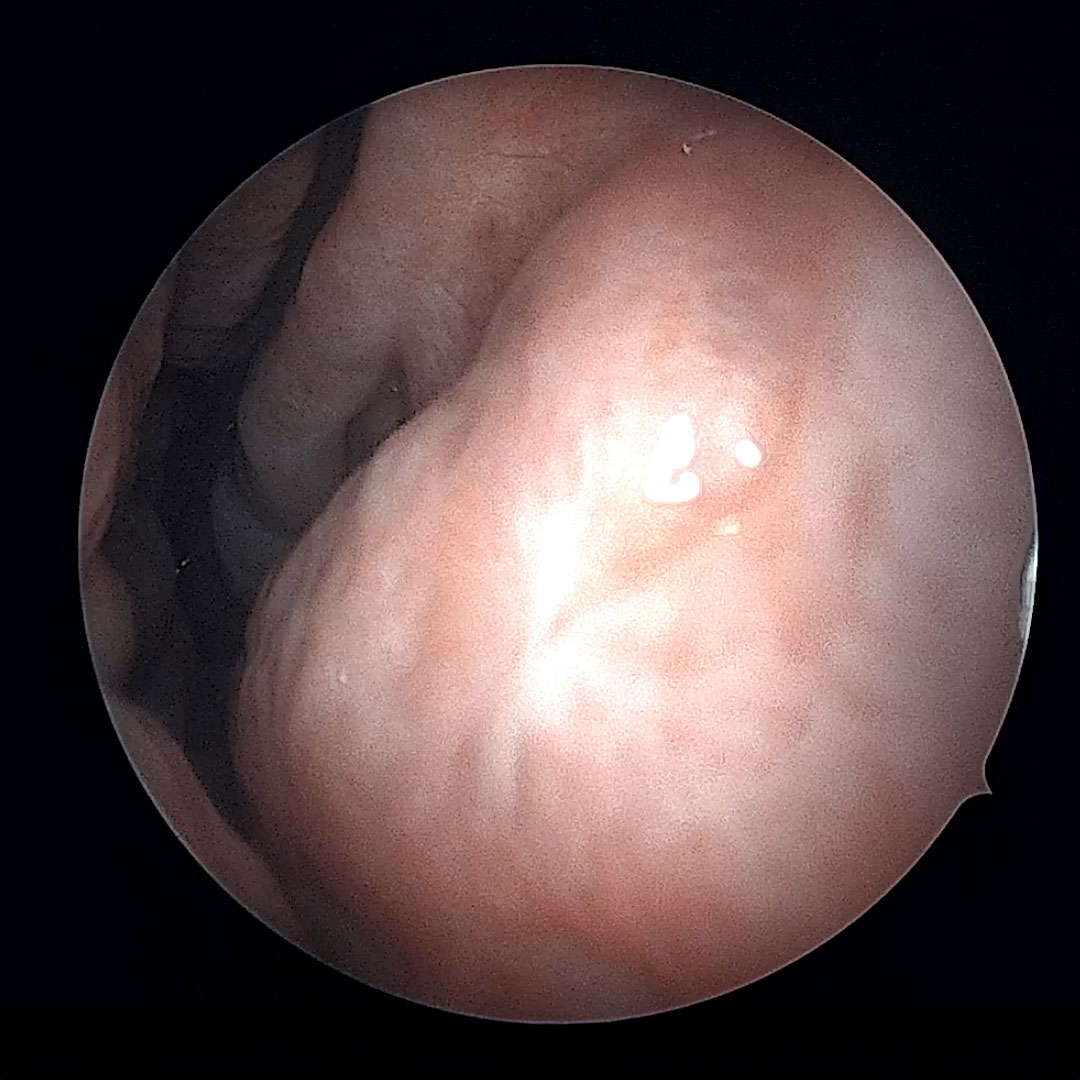 After
AfterPatient’s Perspective
Surgical Repair of Empty Nose Syndrome
Five years ago, Mablean Warren had surgery for a deviated septum and enlarged turbinates. Initially, she did every well, but then she noticed a gradual reduction in her quality of life. ““It was a gradual worsening. After a few months, my nose and head began to feel stuffy all the time, and I couldn’t sleep well because I couldn’t breathe,” says Warren. “I felt like I was suffocating and lost my ability to concentrate. I was irritable and had a lot of anxiety.”
Martin J. Citardi, MD diagnosed her with Empty Nose Syndrome and performed a turbinoplasty procedure on each side. Almost immediately, Warren noticed a big improvement. “It was like, ‘Oh, wow! I can breathe,” she says. “Now I wake up and swing my legs out of bed and say, ‘Watch out world, here I come! Let’s get the party started.”
For more information about Mablean Warren’s story, please see her ORL Notes post.

A little over a decade ago, Giovanni Ordonez started having trouble breathing at night, disrupting his sleep. He saw a local ENT, who recommended turbinate reduction, a procedure that reduces the volume of turbinate tissue to open the nasal airway.
In summer 2021, an ENT referred him to Martin J. Citardi, MD, professor and chair and Memorial Hermann Chair in the Department of Otorhinolaryngology at McGovern Medical School at UTHealth Houston, who suspected empty nose syndrome (ENS). To identify candidates for surgery, Dr. Citardi uses a validated patient questionnaire and the in-office cotton test. “We place a small piece of cotton in the area with missing tissue and ask patients if they perceive a difference,” he says. “If they do, we know they are likely candidates for turbinoplasty. We use the cotton test results to determine where to repair the turbinates.”
For more information about Giovanni Ordonez’s story, please see his ORL Notes post.
Management of Post Surgical
Empty Nose Syndrome
Jason Talmadge, MD and Martin J. Citardi, MD (both from UTHealth Houston) partnered from Jayakar Nayak, MD (Stanford University) in a peer-reviewed review article on Empty Nose Syndrome. In this article, which was published in Facial Plastic Surgery Clinics of North America, they highlight 5 important points:
- Empty Nose Syndrome is most often seen when turbinates are cut and removed but can rarely happen in less invasive surgery.
- The cause of Empty Nose Syndrome is believed to be damaged “cool air” receptors in the nose as well as loss of nerve fibers that sense breathing.
- The loss of airflow sensation can cause significant anxiety and depression symptoms that often need to be addressed along with rebuilding nasal tissue.
- Using a standardized survey and the “cotton test” an experienced physician can develop a plan to treat and sometimes cure Empty Nose Syndrome.
- If medications and office procedures do not provide enough relief, surgery can be performed to attempt to restore normal airflow with grafts placed under the nasal lining to mimic the lost turbinates.
For more info, please see the publication abstract.


Martin J. Citardi, MD
Martin J. Citardi, MD, an internationally recognized rhinologist, currently serves as Professor and Chair of the Department. Dr. Citardi received his doctor of medicine degree from The Johns Hopkins University School of Medicine. He completed his residency training at Yale University and then pursued a rhinology fellowship at the Georgia Rhinology & Sinus Center. Dr. Citardi is certified by the American Board of Otorhinolaryngology, and he is a fellow of the American Academy of Otolaryngology, the American College of Surgeons and the American Rhinologic Society.
UT Physicians Otorhinolaryngology – Texas Medical Center
Houston, TX, 77030-1539
Xiaoyang Hua, MD, PhD, is a board-certified otorhinolaryngology specialist and researcher. He’s also an associate professor of Otorhinolaryngology-Head and Neck Surgery at UTHealth Houston.
Hua received his medical degree from Tongji University School of Medicine and his doctorate from Tongi Medical University. He completed his residency and a fellowship program at the University of Iowa Hospitals and Clinics.
UT Physicians Otorhinolaryngology – Texas Medical Center
Houston, TX 77030-1539
(713) 486-5000
Treatment Options
Medical Therapy
This is usually our first method of treatment. Our doctors may recommend a variety of nasal sprays and ointments to improve nasal dryness and blockage. Prior to your visit, we recommend the use of a humidifier and saline sprays to increase moisture, which often helps with symptoms.
In-office Procedures
Certain issues can be relieved with minor procedures performed in the office. During your evaluation, you can determine if this option is best for you.
Surgical Procedures
Some patients require surgery to rebuild the lost tissue from prior nasal procedures. Thanks to medical advancements, a variety of safe and effective materials can be used to replace the missing tissue.




