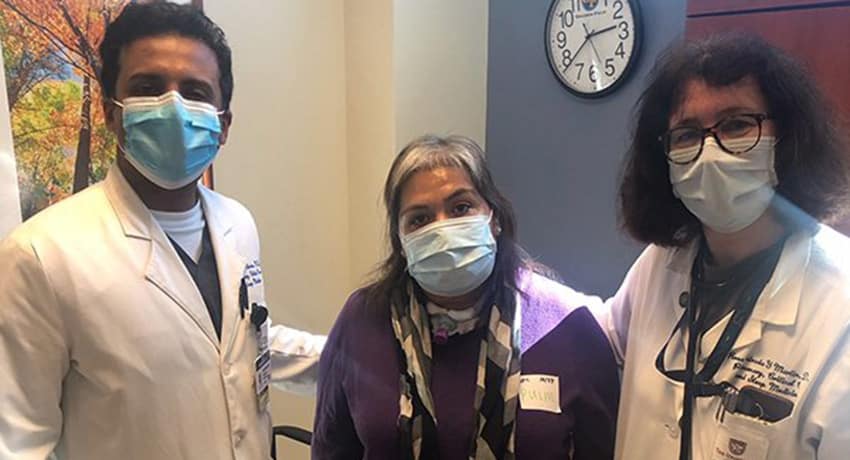
Elizabeth Silva, 47, is more grateful than ever to spend time with her family this year – just last year she couldn’t move or speak after spending weeks in an intensive care until (ICU) battling COVID-19.
“I really didn’t know if I was going to survive,” Silva said. “The virus took everything from me, mentally and physically. Doctors and physical therapists had to teach me to get up, walk, shower, and even brush my hair.”
In mid-June she started having flu-like symptoms, but none of the usual treatments for flu were working. She was rushed by ambulance to Harris Health’s Lyndon B. Johnson Hospital, where she would spend the next two months.
“When I got to the hospital, they gave me oxygen and within five minutes, I fell unconscious. I don’t remember anything that happened for the next few weeks,” she said.
However, the physicians from The University of Texas Health Science Center at Houston (UTHealth) who helped Silva fight for her life at Harris Health LBJ will never forget what happened during that time.
“She was very sick – sedated on a ventilator and completely paralyzed for weeks,” said Rosa Estrada-y-Martin, MD, professor of medicine with McGovern Medical School at UTHealth and medical director of pulmonary and critical care medicine at Harris Health LBJ. “We’d put her in the prone position for 16 hours a day to give the lungs a chance to heal. There were extremely long days for several weeks while we were trying to her oxygen levels to improve. We monitored the ventilator so closely to make sure we were supporting her oxygen levels well enough without damaging her lungs in the process. That’s the challenge.”
The critical care physicians and medical staff monitored the air flow and pressure from the ventilator, ensuring the machine would not cause more harm than good.

“She had severe acute respiratory distress syndrome, where fluid accumulates in your lungs,” said , Sujith Cherian, MD, assistant professor of medicine at McGovern Medical School and director of quality for pulmonary and critical care medicine at Harris Health LBJ. “Air hunger can develop in patients with lung inflammation that causes them to breathe in a way that is out of sync with the ventilator and can cause severe lung damage. So to prevent that, we prescribed strong sedatives and paralytics to induce a deep sleep. At one point, her oxygen levels dropped and carbon dioxide levels rose too high and I really thought she wasn’t going to make it. Multiple rounds of the prone position, adequate ventilator support, appropriate medications, and protecting her from infections with safe practices in the ICU went a long way to save her.”
Estrada-y-Martin and Cherian said Silva likely survived because they were able to prevent infections, which are common in severe COVID-19 patients, and kidney function remained normal throughout her time in the ICU.
Silva also received convalescent plasma to provide her with antibodies to fight the infection and medication to keep her blood from clotting. When she regained consciousness in mid-August, she had a whole host of new challenges to overcome.
“When I woke up, I could not speak, move, or walk,” Silva said. “Even moving my arms was very hard and I was in shock from it. I arrived at the hospital being able to move around freely and suddenly I was dependent on everyone.”
She had a breathing tube inserted in her windpipe to allow her lungs to continue to heal. She was also dealing with myopathy, which is muscle and nerve weakness that is common after a long ICU stay, Estrada-y-Martin said.
Physical therapy helped Silva regain movement, but she is still recovering from the toll COVID-19 left on her mental health.
“This virus leaves you very depressed and emotionally vulnerable,” Silva said. “It’s something really hard for me to explain because I have never experienced this type of depression and constant fear of being reinfected. But I still have hope to try to go back to work and get back to normalcy with my regular life.”
In late November, she had the breathing tube removed, and now she’s back to being able to engage in the hobbies she loves: cooking, reading, and spending time with her family.
“She’s completely independent now, which is amazing since previously she couldn’t even move a finger. Her case is a bright spot in this pandemic,” said Estrada-y-Martin, who also sees pulmonary patients at UT Physicians.
“The best part of being a pulmonary and critical care physician is to see patients survive and come out of ICU. We’ve been following Silva in clinic and it’s been great to see her improvement. We had a completely concerted effort between the physicians, nurses, physical therapists, rehabilitation therapists, nutritionists, clinical pharmacists, residents, and fellows – a really good team that helped take care of her, and without all that, she likely wouldn’t be where she is,” Cherian said.