Placenta Accreta Program at UTHealth Houston
Maternal-fetal medicine specialists provide expert care for high-risk pregnancy complications involving the placenta.
Placenta Accreta Program at UTHealth Houston
Maternal-fetal medicine specialists provide expert care for high-risk pregnancy complications involving the placenta.
Coordinated Care for You and Your Baby
The Placenta Accreta Program at UTHealth Houston offers a multidisciplinary team of board-certified specialists who help mothers with placenta accreta spectrum (PAS) disorder. Our experts provide a full spectrum of services, including prenatal testing, diagnostic imaging, and specialized maternal-fetal care.
What is placenta accreta spectrum (PAS) disorder?
This is a complex condition where the placenta does not entirely detach after birth and cannot be removed without causing significant risks to the mother.
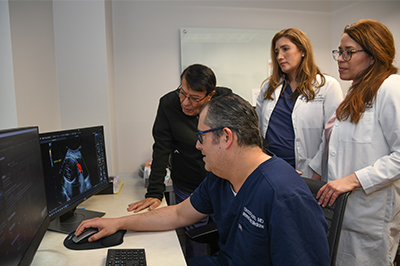
Early Detection and Diagnosis
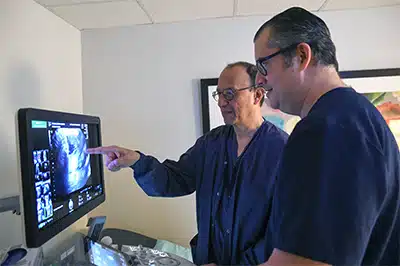
PAS disorder is an infrequent placental anomaly, usually diagnosed during the mid-trimester anatomy ultrasound at 18 to 22 weeks of pregnancy, but it may be discovered later, including at delivery. The quicker our team can diagnose the condition, the sooner we can minimize the risk of complications during delivery.
Diagnosis
Patients who have been diagnosed with placenta previa, had multiple C-sections, or undergone uterine surgeries are at risk for this life-threatening condition. Our medical team employs state-of-the-art imaging and sonar technology to precisely diagnose placenta accreta. We conduct routine imaging throughout pregnancy and post-delivery to optimize outcomes.
Treatment Options
Three options for treatment offered at UTHealth Houston are C-section and hysterectomy, delayed hysterectomy, or keeping the uterus for a potential future pregnancy. You will be counseled on the risks and benefits of each approach.Cesarean hysterectomy with bilateral salpingectomy
According to the American College of Obstetricians and Gynecologists, the generally accepted approach to placenta accreta spectrum is a cesarean hysterectomy with the placenta left in place after delivery. Attempts at placenta removal are associated with a significant risk of hemorrhage.
Leaving the placenta in situ with delayed hysterectomy
If the placenta invades the bladder or surrounding tissues, delaying the hysterectomy allows time for the accreta to shrink, lessening the risk of potential injury to other organs, bleeding, and admission to the intensive care unit.
Leaving the uterus and placenta in situ
Some patients opt for potential future fertility. We counsel them extensively about the importance of follow-up. We continue to monitor them after delivery for signs of infection or bleeding, which are risk factors, while the placenta shrinks and reabsorbs. With our expert team and streamlined process, we can act quickly if there is any reason for concern. This is an important option for women who want to keep their uterus for a potential future pregnancy, or for cultural or religious reasons. We always advise that we may need to do a hysterectomy, depending on what happens during the delivery.
Immediate Access to Critical Care
If PAS is not diagnosed prior to delivery and the team identifies placental invasion of the bladder and other organs, we advise immediate closure of the abdomen and prompt evaluation by our specialists. We are equipped to address the health needs of both you and your baby.
Our PAS care team includes maternal-fetal medicine specialists, sonographers and radiologists specialized in fetal and maternal imaging, anesthesiologists, neonatologists, gynecologic oncologists, inpatient and outpatient nurse navigators, a skilled labor and delivery team, and blood bank access. We closely monitor and provide compassionate care throughout your pregnancy and delivery.
Our program maintains continued communication with referring primary obstetricians to keep them informed about patient progress throughout the delivery and follow-up process. After complete resolution, referring physicians receive a summary and a plan for follow-up care. The team encourages continued communication with each patient during and after treatment.
Patient Stories
Specialists
Maternal-Fetal Medicine
Maternal-Fetal Medicine
Maternal-Fetal Medicine
Maternal-Fetal Medicine
Maternal-Fetal Medicine
Edgar A. Hernandez-Andrade
MD, PhD
Maternal-Fetal Medicine
Maternal-Fetal Medicine
Gynecology Oncology
Gynecologic Oncology
Gynecologic Oncology
Anesthesia

Jennifer Hoayek, MD
Obstetric Anesthesiology

Barbara Orlando, MD, PhD
Obstetric Anesthesiology
Nurse Navigator

Holly Howington, RN
Nurse Navigator
Locations
Houston, TX 77030-3002
Mon - Fri 8 a.m. - 5 p.m.
Houston, TX 77030-3004